Written by Aidan Lunney – APA Sports & Exercise Physiotherapist
Over the last 10 years, the spotlight has certainly shone bright on acute head injuries, or as we know it – Concussion. Prior to this, it was often brushed to the side, seen as a badge of toughness and an injury that wasn’t taken seriously because the damage wasn’t visible. Having previously worked in schoolboy level, and now semi-professional state level Rugby League, the scary reality that is a concussion, or to be specific, a Traumatic Brain Injury and it’s frequency has never been more pertinent to me. This year has seen the Australian Institute of Sport, in conjunction with the Australasian College of Sports & Exercise Physicians, Australian Physiotherapy Association and Sports Medicine Australia release the “2024 Concussion and Brain Health Position Statement”. The importance of recognition, assessment and the role of appropriate rehabilitation was highlighted, particularly with a spotlight on the effectiveness of Physiotherapy intervention in managing and assisting in the return to play and performance process. This topic is what we will look to unpack and highlight in this blog piece, a topic that is a keen interest area of mine.
What is a Concussion?
A concussion is defined by the American Association of Neurological Surgeons (2024) as “an injury to the brain that results in temporary loss of normal brain function. Medically, it is defined as a clinical syndrome characterised by immediate and transient alteration in brain function, including alteration of mental status or level of consciousness, that results from mechanical force or trauma.” Often, impairments in memory, judgement, reflexes, balance and muscle co-ordination are seen, or the individual reports a brief period fogginess or confusion, Concussions are often seen in large head collisions, however can also be more innocuous, requiring a high level of suspicion for everyone involved. Regardless of the severity or presentation, all head trauma should be taken seriously, considering current commentary and findings of Chronic Traumatic Encephalopathy (CTE) which is a degenerative brain disease resulting from recurrent head trauma.
How do we recognise a Concussion?

A concussion can be recognised by the following signs and symptoms:
- High Velocity or Direct Head Collision
- Confusion
- Headache
- Vision disturbances (double or blurry vision)
- Dizziness or imbalance
- Nausea or vomiting
- Memory loss
- Ringing ears (Tinnitus)
- Difficulty concentrating
- Sensitivity to light
- Loss of smell or taste
- Trouble falling asleep
Duration of Concussion Symptoms
What a tough question to answer! Current evidence tells us that physiological healing of our brain post a concussive episode is near complete at three week point post injury. However, despite these timeframes, we often see an array of longer lasting deficits following a concussive episode. People dealing with post-concussion syndrome, or longer lasting concussive symptoms continue to deal with symptoms related to:
- Light and sound irritability
- Balance and Vestibular issues
- Short and Long Term Memory issues
- Cognitive dysfunction
- Autonomic Nervous System Dysfunction – e.g. fatigue and exercise intolerance
- Neck and upper back pain
- Headaches
- Gaze stability and visual focus – difficulty with visual focus in both simple and complex scenarios.
What is the current management of a concussive episode?
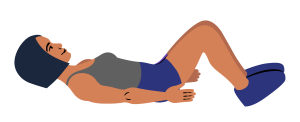
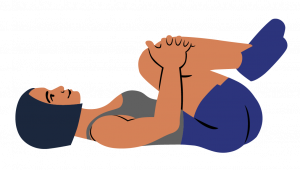
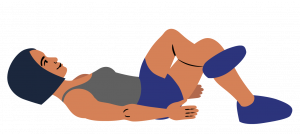
Whilst sporting governing bodies across the globe adopt slightly variable management and return to play processes, it is important to understand and be aware of the core stages in managing a concussion, and subsequently safely returning to play. Variability presents itself across sporting codes policies when it comes to timeframes for graduated return to training stages and subsequent play. Following appropriate physical, cognitive and emotional rest, a graduated return to low intensity, followed by high intensity sport-specific training occurs. This occurs in conjunction with targeted rehabilitation that as Physiotherapists, we employ to target key areas such as balance, visual and neck/upper back impairments should they arise.

How can Physiotherapy help with post-concussion symptoms?
Physiotherapy guided rehabilitation can be extremely effective in managing the spectrum of effects that are resultant of a concussion. Physiotherapist’s are well versed in concussion specific assessment, diagnosis and holistic rehabilitation. Patient and contextually specific advice and education, targeted manual therapy and deficit specific rehabilitation in a patient specific, multi-disciplinary model is our approach here at Physioactive. With assistance from our Sports Registrar, Dr. Jack Cookson, who has a keen interest in concussion rehabilitation and can assist in timelines and return to work/play processes, we aim to work collaboratively with our patients in delivering an evidenced based, contemporary and patient specific rehabilitation profile. In this, ensuring a safe, progressive and all-encompassing return to performance profile occurs, exemplified in the diagram on the right.
How can we help you at Physioactive?
Offering a full suite of Sports Medicine and Allied Health Services, we at Physioactive are best placed to assist with your concussion management. To make an appointment, or for more information, please give us a call on 3281 8876 or visit our website at www.physioactive.com.au
References & Resources
2024 Concussion and Brain Health Position Statement – https://www.concussioninsport.gov.au/__data/assets/pdf_file/0004/1133545/37382_Concussion-and-Brain-Health-Position-Statement-2024-FA.pdf